164 J.SASI HARSHITH ELOG CASES
A 50 Year Old Female with Tuberculosis?
J.SASI HARSHITH
Roll No. 164
A 50yr old female came with c/o shortness of breath (Grade 2) since 25 days.
C/o Difficulty in swallowing solids and liquids since 8 days.
C/o Difficulty in walking and movement since 8 days
History of Presenting Illness :
Pt was apparently alright 10 years ago then she got severe headaches, and was easily fatigued, and on a visit to hospital for it she was diagnosed with hypertension and started on medications since then.
6 years ago hospital in view of weight gain and easy fatigability, she visited hospital and was diagnosed with Hypothyroidism and started on medications for it since then.
Later she was diagnosed with Arthritis but is not on any medications.
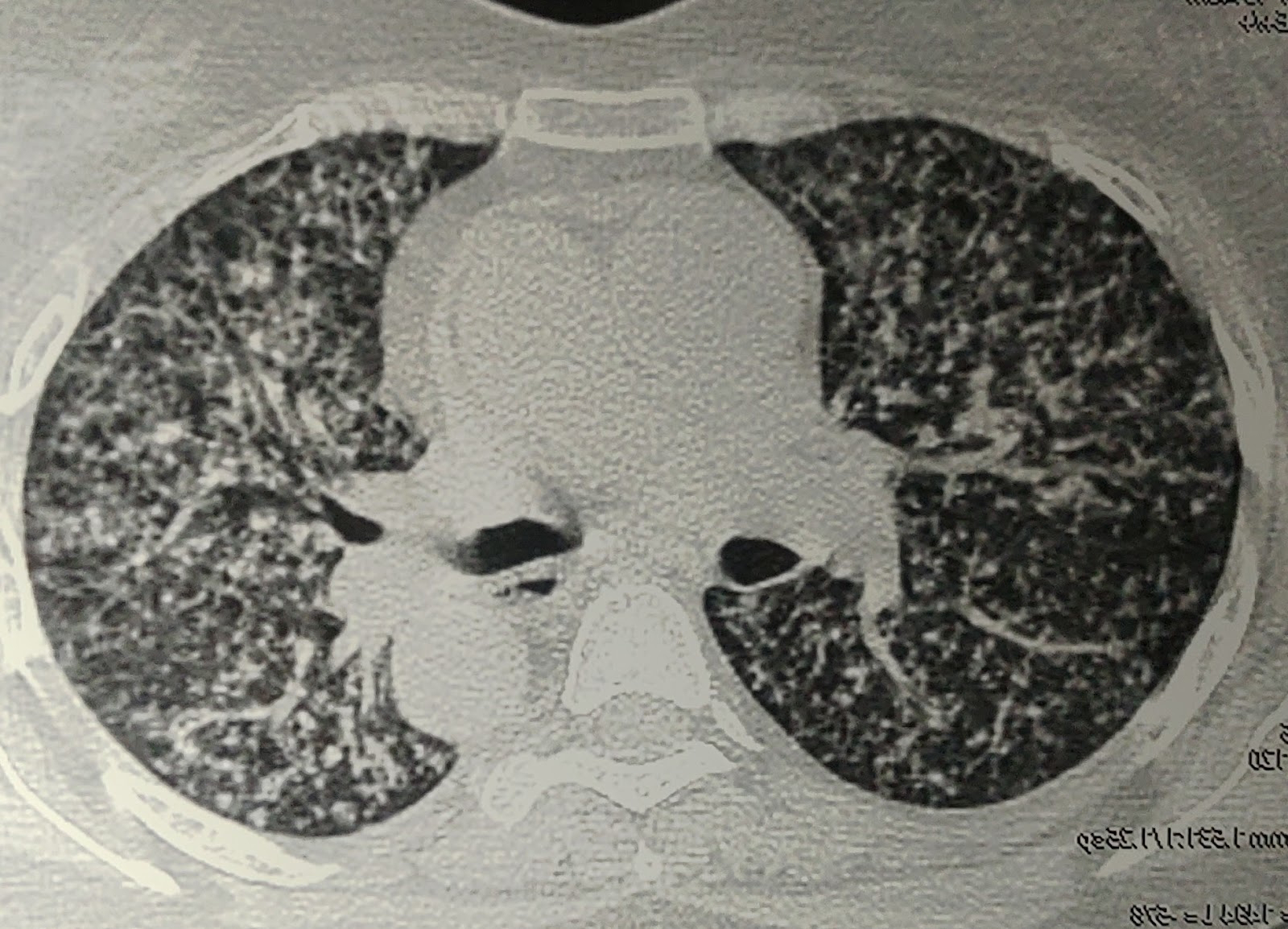
2 months back Pt had C/o cough with expectoration, pain in chest region. was diagnosed as PULMONARY MILIARY TB based on Chest X Ray and started on ATT. After 1 month of use she started developing redness and itching all over the body ATT induced Erythroderma, stopped ATT on 1 Feb 2022 for 20 days.
She was then shifted to a Government Hospital. There she stopped her ATT and was treated for her cutaneous condition. She again started having SOB ( grade 2), not associated with any Orthopnea/ Paroxysmal Nocturnal Dyspnea, Pedal Edema, Chest Pain, or Palpitations.
From 5 days she has difficulty in swallowing solids and liquids and was had difficulty in swallowing solids and liquids and was having difficulty in opening of mouth because of pain and c/o reddish discoloration of the tongue but now it got reduced.
Past History:
k/c/o De novo Diabetes since 3 months, (Not on Medication)
k/c/o Hypertension since 3 years (on Medication- Amlodipine 5mg)
k/c/o Pulmonary miliary TB on ATT using 3 Tablets/ day (H- Isoniazid, R- Rifampicin, Z- Pyranzinamide, E- Ethambutol)
k/c/o Hypothyroidism since 6 years on Thyronorm 50 mcg.
Personal History:
- Decreased appetite
- Mixed diet
- Sleep Normal
- Bowel and Bladder-
- Addictions-
On Examination:
Patient was examined in a well lit room after taking consent her consent.
- The Patient was conscious, coherent and co operative. She was well oriented to time, place and person
- NO Cyanosis/ Clubbing/Lymphadenopathy
- PALLOR +
- ICTERUS+
- Temperature:100F
- PR: 98bpm
- BP:130/80mm Hg
- RR:27cpm
- Spo2: 95%
- GRBS:105gm%
Systemic Examination:-
- CVS: JVP NORMAL, Apex beat 5th IV space mid clavicular line; s1 s2 +
- RS: BAE + , B/L crepts + (ISA, IAA)
- P/A: soft, non tender , BS +
- RBS: 70mg/dl
- HbA1c : 6.8%
- RFT
Blood Urea: 136mg/dl
S. Creatinine: 4.8mg/dl
Na -139
K - 3.0
Cl - 102
- Hemogram
Hb - 7.2
TLC - 15,000
MCV - 80.4
PCV - 21.5
MCH - 27.0
MCHC - 33.6
PLT - 3.67
RDW - 62
Peripheral Smear: NORMOCYTIC, NORMOCHROMIC
Serum iron : 45ug/dl
- ABG
pH - 7.34
PCo2 - 18.8
PaO2 - 92.4
HCO3 - 12.2
SpO2 - 96
- LFT
TB - 2.8
DB - 0.74
AST - 14
ALT - 10
ALP - 673
TP - 7.4
ALB - 2.23
- CUE
ALB - ++
Sugars - nil
Pus cells - plenty
Epithelial cells - 1-2
- COVID-19 Rapid Antigen Test - NEGATIVE
- ESR - 70
- CRP - POSITIVE
- Chest X-Ray
- X- Ray Neck (Lateral view)
- Small air filled cyst noted left lower lobe.
- No evidence of effusion.
- Non-obstructive left renal culculus.
- IVF NS/RL/DNS @ 75 ml/hr
- Inj. NaHCO3 50meq over 10 mins + 50meq over 40 mins
- NEB. Ipravent 1resp inH TID
- NEB. BUDICORT 1RESP INH TID
- INJ. HUMAN ATRAPID according to sliding scale
- Amlodipine 5mg PO OD
- Inj. PIPTAZ 2.25 gm IV TID
- T. Thyronorm 50 mg PO OD
- INJ. PAN 40 MG IV OD
- T. AMLONG 5 MG PO OD
- MUCOPAIN GEL L/A 40 MINS BEFORE MEAL
- Betadine mouth wash TID
- Liquid paraffin all over body TID
- IVF- NS,RL: urine output + 30ml/hr
- Inj. PIPTAZ 2.25gm IV TID
- Neb IPRAVENT 1 resp INH TID
- Neb BUDECORT 1 resp INH TID
- Inj. HUMAN ACTRAPID acc to GRBS
- GRBS monitoring 6 th hrly
- T. THYRONORM 50ug PO OD
- Inj. PANTOP 40mg IV OD
- T. Amlong 5mg PO OD
- MUCOPAIN GEL for L/A ( 10 mins before each meal in oral cavity)
- BETADINE mouth wash TID
- LIQUID PARAFFIN all over the body TID
- STOP ATT
- strict I/o charting, temperature charting every 4th hrly
- Get link
- X
- Other Apps
- Get link
- X
- Other Apps